Diastolic dysfunction is a condition that affects the ability of the heart to relax and fill with blood during its resting phase, also known as diastole. This condition can lead to a variety of symptoms and complications, including heart failure, arrhythmias, and reduced exercise capacity. In this article, we will explore the causes, symptoms, and treatment options for diastolic dysfunction.

What is Diastolic Dysfunction?
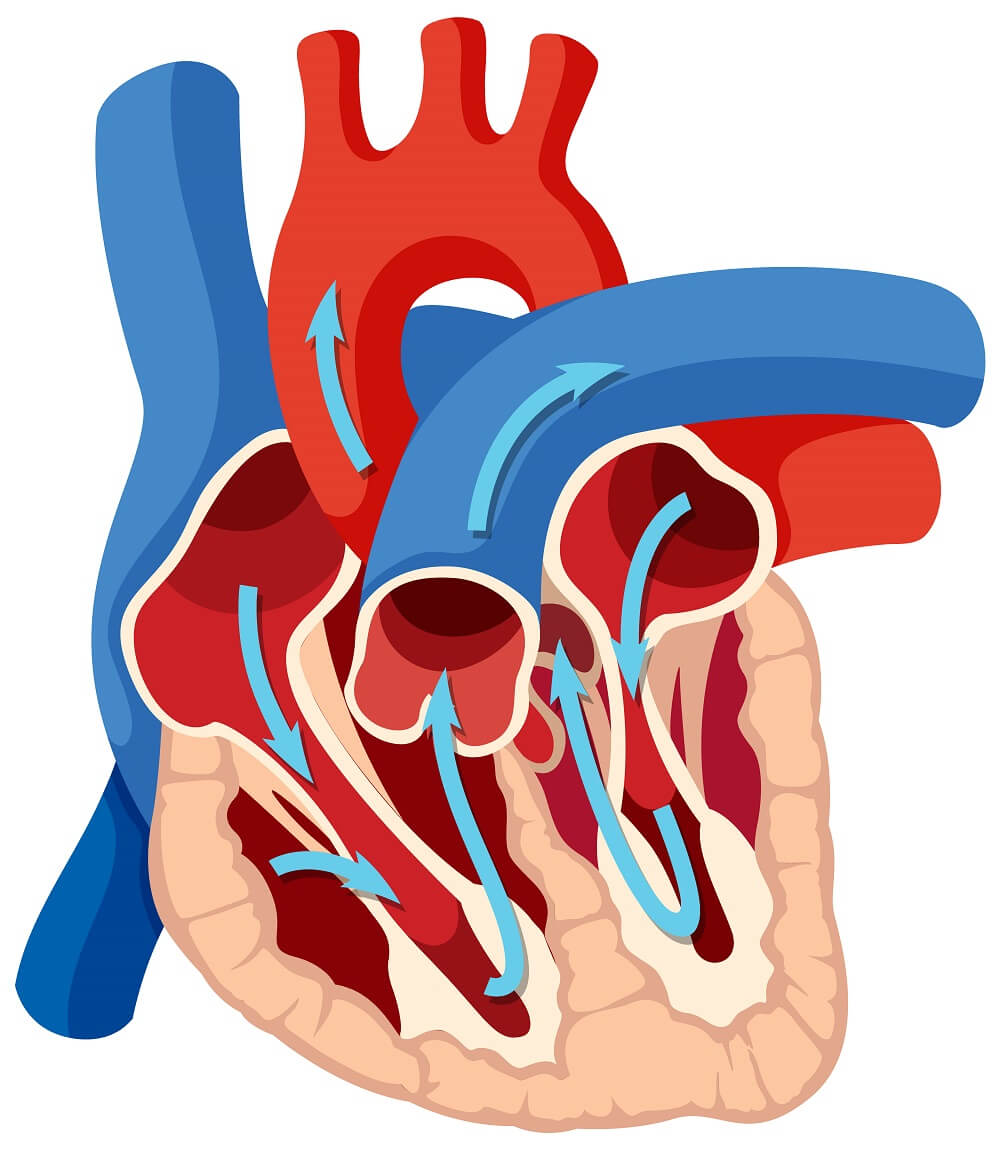
Diastolic dysfunction is a condition in which the heart is unable to relax and fill with blood during its resting phase, leading to impaired diastolic function. This means that the heart cannot effectively pump blood throughout the body, resulting in a range of symptoms and complications.
Grades of Diastolic Dysfunction
There are two main types of diastolic dysfunction grades: grade I, which is mild dysfunction, and grade II-IV, which is severe dysfunction.
Causes of Diastolic Dysfunction
Diastolic dysfunction can be caused by a variety of factors, including hypertension, obesity, diabetes, coronary artery disease, valvular heart disease, and aging. Other potential causes include myocardial ischemia, restrictive cardiomyopathy, and infiltrative diseases such as amyloidosis.
Risk Factors for Diastolic Dysfunction
Several risk factors have been associated with an increased risk of developing diastolic dysfunction, including age, hypertension, obesity, diabetes, smoking, and a sedentary lifestyle. Additionally, certain medical conditions such as myocardial infarction, valvular heart disease, and atrial fibrillation can also increase the risk of developing diastolic dysfunction.
Signs and Symptoms of Diastolic Dysfunction
The symptoms of diastolic dysfunction can vary depending on the severity of the condition. Some common symptoms include
- Shortness of breath
- Fatigue
- Swelling in the legs or ankles, and
- Chest pain
In severe cases, patients may experience heart palpitations, syncope, and decreased exercise tolerance.
Diagnosis of Diastolic Dysfunction
Diagnosing diastolic dysfunction typically involves a combination of medical history, physical examination, and diagnostic tests. These tests may include
- Echocardiography,
- Electrocardiography (ECG)
- Stress testing, and
- Cardiac catheterization
Treatment Options for Diastolic Dysfunction
There are several treatment options available for diastolic dysfunction, including lifestyle changes, medications, and surgical or interventional procedures. These may include weight loss, regular exercise, smoking cessation, medications to control blood pressure and heart rate, and surgical procedures such as valve replacement or coronary artery bypass grafting.
Lifestyle Changes for Diastolic Dysfunction
Lifestyle changes can be an effective way to manage and improve diastolic dysfunction. These changes may include maintaining a healthy weight, quitting smoking, getting regular exercise, reducing salt intake, and limiting alcohol consumption.
Surgical and Interventional Treatments for Diastolic Dysfunction
In some cases, surgical or interventional treatments may be necessary to manage diastolic dysfunction. These may include valve repair or replacement, coronary artery bypass grafting, percutaneous coronary intervention, or implantable devices such as pacemakers or defibrillators.
Prevention of Diastolic Dysfunction
While not all cases of diastolic dysfunction can be prevented, there are steps that can be taken to reduce the risk of developing this condition. These may include maintaining a healthy weight, controlling blood pressure and cholesterol levels, quitting smoking, and getting regular exercise.
Frequently Asked Questions (FAQs)
Q1. Can diastolic dysfunction be cured?
A1. While diastolic dysfunction cannot be cured, it can be managed with appropriate treatment and lifestyle changes.
Q2. Can diastolic dysfunction lead to heart failure?
A2. Yes, diastolic dysfunction can lead to heart failure if left untreated or poorly managed.
Q3. Is diastolic dysfunction more common in men or women?
A3. Diastolic dysfunction is more common in women than men, particularly in postmenopausal women.
Q4. Can exercise worsen diastolic dysfunction?
A4. In some cases, intense exercise may worsen symptoms of diastolic dysfunction. However, regular moderate exercise can be beneficial for managing this condition.
Q5. Can diastolic dysfunction be prevented?
A5. While not all cases of diastolic dysfunction can be prevented, maintaining a healthy lifestyle and managing risk factors can help reduce the risk of developing this condition.
Conclusion
Diastolic dysfunction is a condition that affects the ability of the heart to relax and fill with blood during its resting phase. While this condition can be serious and lead to complications such as heart failure, it can be managed with appropriate treatment and lifestyle changes. If you experience symptoms of diastolic dysfunction, such as shortness of breath, fatigue, or chest pain, it is important to seek medical attention promptly to receive an accurate diagnosis and appropriate treatment.
Also, read:
Heart Failure Symptoms: Understanding the Signs and Seeking Treatment
Silent Heart Attack: Symptoms, Risk Factors, Prevention, and Treatment